Geriatric nurse practitioner Alice Bonner discusses the special considerations that arise for older adults living in long-term care facilities during the COVID-19 pandemic
More than 400 nursing homes and long-term care facilities in the United States are now also hotspots for person-to-person transmission of COVID-19. Many of these facilities are located in large cities such as New York City and Los Angeles, but the disease isn't contained to urban centers. In Maryland, 77 of the 95 residents in a Mount Airy nursing home have tested positive for the coronavirus, and five residents have died of complications from the disease.
Alice Bonner is a geriatric nurse practitioner who has served as director of the Division of Nursing Homes in the Centers for Medicare and Medicaid Services. She is a senior adviser with the Institute for Healthcare Improvement and an adjunct faculty member at the Johns Hopkins School of Nursing. She joined Sarah LaFave, a PhD student at the Johns Hopkins School of Nursing, to discuss the special considerations that arise for older people living in long-term care facilities during the COVID-19 pandemic. The conversation has been edited for length and clarity.
There is a great deal of concern about the spread of COVID-19 in long-term care settings. Why are these settings at heightened risk for outbreaks?
Older people and people with multiple co-morbidities tend to have more severe symptoms if they contract COVID-19. Residents of nursing homes tend to be more frail, have more functional limitations, and have more chronic and complex conditions than other older adults. Based on the data that we have about COVID-19, that puts nursing home residents at highest risk for serious illness as a result of exposure.
In addition, nursing home residents often require help with things like using the toilet, getting in and out of bed, and getting dressed. Social distancing and hand-washing are the best ways to prevent spread of the virus, but these essential person-to-person interactions are still going to have to happen, meaning that residents and staff may be more likely than other people to spread the virus to one another.
What precautions are long-term care facilities taking to limit the spread of COVID-19?
Pretty much across the board, facilities are limiting visitors. For the most part, the only people who should be going into nursing homes and assisted living facilities at this point are essential staff. There are a few exceptions to that, such as in the case of compassionate care. If someone is not expected to live many more days or weeks, a family member may be permitted to visit. Also, for some people who have behavioral manifestations of dementia, for example, it may be necessary to permit a familiar one-on-one caregiver to be with that person.

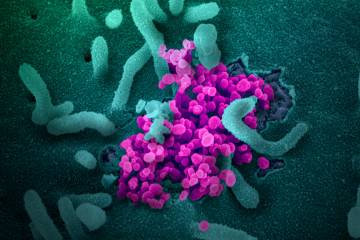
Image caption:The Life Care Center of Kirkland in Washington became the epicenter of the state's outbreak of coronavirus in early February, when 81 of 120 residents tested positive for COVID-19 and 34 died from the illness.
IMAGE CREDIT: GETTY IMAGES
Another thing that facilities are doing is screening staff and essential visitors for symptoms of COVID-19. That might include taking a person's temperature and asking about recent respiratory symptoms like a cough and shortness of breath, before that person enters the facility. In addition, facilities are providing meals to residents in their individual rooms rather than in group settings, and have canceled group activities.
Who makes decisions about visitor policies and other precautions for long-term care facilities?
The Centers for Disease Control and Prevention and CMS put out federal guidance. In addition, each state health department, or whatever other state agency oversees nursing home safety and quality in a particular state, will issue state-specific recommendations or mandates. These typically include guidance on visitation policies, hand-washing, use of personal protective equipment, use of private rooms and isolation, testing procedures, and disease management.
If an older person in a nursing home develops COVID-19 symptoms right now, how are facilities handling that?
The answer is not to take the person directly to the emergency room or to call 911, unless the person has emergent symptoms like trouble breathing. The resident or a nursing home representative should communicate with the resident's primary care provider as a first step. In addition, the resident should isolate in a private room and personal protective equipment should be used based on CDC guidelines.
Do staff and providers in nursing homes receive ongoing training on infection control? How prepared do you think most residential facilities are to implement precautions or manage the COVID-19 outbreak?
Federal and state regulations typically require that infection prevention, surveillance, and management be part of new staff orientation and ongoing quality assurance and improvement efforts. With that said, the inspector general recently reported that infections are one of the primary adverse events that occur in nursing facilities. Infection control in long-term care settings is a concern that has existed for years, and the current outbreak is bringing it into sharper focus.
ALSO SEE
One urgent concern in terms of preparedness is the potential for workforce shortages. As the likelihood of a surge in cases approaches, it will become even more critical to identify individuals who are not contagious, since we may need to train additional health care workers to supplement the hospital, home care, and long-term care workforce. Some states are working on innovative methods to quickly train people who are out of work to become part of this workforce. In order to do that, states are asking the federal government for emergency waivers of federal requirements to help expedite training.
All the precautions we've talked about make sense from an infection-control perspective, but I imagine they also present a host of concerns about resident well-being.
Older people may experience anxiety or even depression due to social isolation during this time of social distancing. We need to be creative in safely providing opportunities for human interaction. Friends and family should consider contacting older people who may be isolated by making a friendly phone call. People can also think about contacting a local nursing home or assisted living residence and offering to make telephone calls to residents or their family members to provide support during this difficult time. There are also a lot of meaningful (including remote) volunteer opportunities available right now through Meals on Wheels, local departments of health, area agencies on aging, nursing facilities, and other organizations that support older people.
In addition to social isolation and loneliness, we're always concerned about elder mistreatment, neglect, and self-neglect. There is an increased risk for those issues right now. If older people, their loved ones, or others have concerns about any of these issues, they can contact their local Adult Protective Services Agency for support. It's OK to report suspected mistreatment even if you don't know for sure that it's happening.
Regardless of where they live, older adults are part of the fabric of our society. We do have to be careful about spreading the virus, but that doesn't mean that we should stop looking out for one another.
Posted in Health, Voices+Opinion