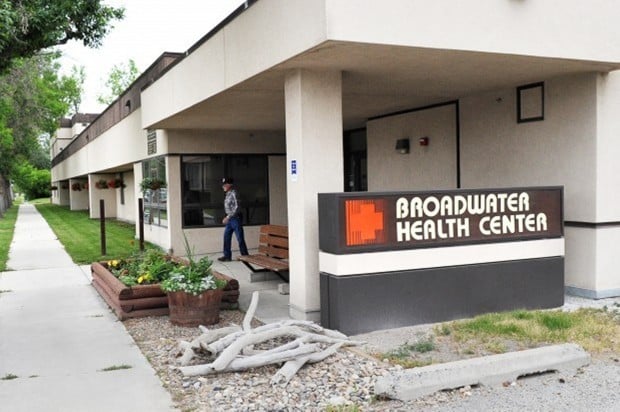
Saturday’s closure of the Broadwater Health Center Nursing Home in Townsend will create a financial strain that could threaten the viability of the center’s 10-bed hospital, according to the center’s board chair.
Joni Carlson, chair of the board of Townsend Health Systems, said cash flow from the 35-bed nursing home helps keep the critical-access hospital and its 24-hour emergency room running. That cash flow ends with the nursing home’s closure, ordered Tuesday by the Montana Department of Public Health and Human Services after the facility’s failure to correct deficiencies the state said placed residents’ health and safety in “immediate jeopardy.”
Without the nursing home, “We cannot support our emergency room and hospital,” Carlson said Friday. “Financially, it’s a very big stretch; I don’t know that we’re going to be able to support it, certainly not for the long term.”
“It is something that we want to get started on right away,” Carlson said. “It’s going to be critical to determine which direction we’re going.”
She said the transition of residents out of the nursing home has been smooth, with excellent work by other nursing homes in the area that are taking some of them.
“It’s just been a really hard day around here for all these folks to say goodbye,” said Davis, who has resigned from her post effective Aug. 15.
Board member Hugh van Swearingen said the displaced residents may not be treated as lovingly at their new homes.
“The upheaval now confronting the displaced residents and their families makes my heart ache,” he wrote. “It seems so unnecessary and bureaucratic.”
On Monday, the board unanimously suspended Campbell from the emergency room for 60 days, citing his failure on four occasions over the weekend to report within 30 minutes of being paged while on call.
In October, the state Board of Medical Examiners fined Campbell $500 for enabling another person to obtain invalid prescriptions for 3,180 doses of Lortab, a painkiller, in 2006 and 2007.
It also ordered him to take a neuropsychological examination to assure he could practice safely, and to receive remedial education on record keeping.
Campbell did not return a call to his practice Friday seeking comment.
Board members interviewed a CEO candidate Thursday and have additional applicants. The center has an interim director of nursing contracted to begin a 26-week contract July 16.
The board also approved new medical bylaws to ensure compliance with the federal Emergency Medical Treatment and Active Labor Act, a law requiring hospitals to accept nearly all emergency patients.
That followed a May incident in which, according to DPHHS documents, a physician on call at the hospital would not see a patient, 16 weeks pregnant and complaining of abdominal pain, instead sending her to St. Peter’s Hospital in Helena, about 40 miles away, and saying that the facility did not serve obstetric patients.
Staff have raised other issues. A physician assistant told the board that a computer system to chart patients “is a mess” and “is sucking the life out of us.”
Staff also told the board Monday that they had discovered past cases of improper billing, related to the incomplete charting of patient records by physicians, which could constitute fraud against Medicare.
