Summary: Deep sleep, also known as non-REM slow-wave sleep, may help reduce memory loss in older adults facing a heightened burden of Alzheimer’s disease. The research indicates that superior amounts of deep sleep can act as a protective factor against memory decline in those with existing high amounts of Alzheimer’s disease pathology, potentially helping to alleviate some of dementia’s most devastating outcomes.
Key Findings:
- Deep sleep, also known as non-REM slow-wave sleep, may help buffer against memory loss for older adults facing a heightened burden of Alzheimer’s disease.
- Disrupted sleep has previously been associated with faster accumulation of beta-amyloid protein in the brain, which is linked to memory loss caused by dementia.
- Superior amounts of deep, slow-wave sleep can act as a “cognitive reserve factor” that may increase resilience against beta-amyloid pathology, indicating the importance of non-REM slow-wave sleep in counteracting some of the memory-impairing effects of beta-amyloid deposits.
Source: UC Berkeley
A deep slumber might help buffer against memory loss for older adults facing a heightened burden of Alzheimer’s disease, new research from the University of California, Berkeley, suggests.
Deep sleep, also known as non-REM slow-wave sleep, can act as a “cognitive reserve factor” that may increase resilience against a protein in the brain called beta-amyloid that is linked to memory loss caused by dementia. Disrupted sleep has previously been associated with a faster accumulation of beta-amyloid protein in the brain.
However, the new research from a team at UC Berkeley reveals that superior amounts of deep, slow-wave sleep can act as a protective factor against memory decline in those with existing high amounts of Alzheimer’s disease pathology — a potentially significant advance that experts say could help alleviate some of dementia’s most devastating outcomes.
“With a certain level of brain pathology, you’re not destined for cognitive symptoms or memory issues,” said Zsófia Zavecz, a postdoctoral researcher at UC Berkeley’s Center for Human Sleep Science. “People should be aware that, despite having a certain level of pathology, there are certain lifestyle factors that will help moderate and decrease the effects.
“One of those factors is sleep and, specifically, deep sleep.”
The research, published Wednesday in the journal BMC Medicine, is the latest in a large body of work aimed at finding a cure for Alzheimer’s disease and preventing it altogether.
As the most prevalent form of dementia, Alzheimer’s disease destroys memory pathways and, in advanced forms, interferes with a person’s ability to perform basic daily tasks. Roughly one in nine people over age 65 have the progressive disease — a proportion that is expected to grow rapidly as the baby boomer generation ages.
In recent years, scientists have probed the ways that deposits of beta-amyloid associate with Alzheimer’s disease and how such deposits also affect memory more generally. In addition to sleep being a foundational part of memory retention, the team at UC Berkeley previously discovered that the declining amount of a person’s deep sleep could act as a “crystal ball” to forecast a faster rate of future beta-amyloid buildup in the brain, after which dementia is more likely set in.
Years of education, physical activity, and social engagement are widely believed to shore up a person’s resilience to severe brain pathology — essentially keeping the mind sharp, despite the decreased brain health. These are called cognitive reserve factors. However, most of them, such as past years of education or the size of one’s social network, cannot be easily changed or modified retroactively.
That idea of cognitive reserve became a compelling target for sleep researchers, said Matthew Walker, a UC Berkeley professor of neuroscience and psychology and senior author of the study.
“If we believe that sleep is so critical for memory,” Walker said, “could sleep be one of those missing pieces in the explanatory puzzle that would tell us exactly why two people with the same amounts of vicious, severe amyloid pathology have very different memory?”
“If the findings supported the hypothesis, it would be thrilling, because sleep is something we can change,” he added. “It is a modifiable factor.”
To test that question, the researchers recruited 62 older adults from the Berkeley Aging Cohort Study. Participants, who were healthy adults and not diagnosed with dementia, slept in a lab while researchers monitored their sleep waves with an electroencephalography (EEG) machine. Researchers also used a positron emission tomography (PET) scan to measure the amount of beta-amyloid deposits in the participants’ brains. Half of the participants had high amounts of amyloid deposits; the other half did not.
After they slept, the participants completed a memory task involving matching names to faces.
Those with high amounts of beta-amyloid deposits in their brain who also experienced higher levels of deep sleep performed better on the memory test than those with the same amount of deposits but who slept worse. This compensatory boost was limited to the group with amyloid deposits. In the group without pathology, deep sleep had no additional supportive effect on memory, which was understandable as there was no demand for resilience factors in otherwise intact cognitive function.
In other words, deep sleep bent the arrow of cognition upward, blunting the otherwise detrimental effects of beta-amyloid pathology on memory.
In their analysis, the researchers went on to control for other cognitive reserve factors, including education and physical activity, and still sleep demonstrated a marked benefit. This suggests that sleep, independent of these other factors, contributes to salvaging memory function in the face of brain pathology. These new discoveries, they said, indicate the importance of non-REM slow-wave sleep in counteracting some of the memory-impairing effects of beta-amyloid deposits.
Walker likened deep sleep to a rescue effort.
“Think of deep sleep almost like a life raft that keeps memory afloat, rather than memory getting dragged down by the weight of Alzheimer’s disease pathology,” Walker said. “It now seems that deep NREM sleep may be a new, missing piece in the explanatory puzzle of cognitive reserve. This is especially exciting because we can do something about it. There are ways we can improve sleep, even in older adults.”
Chief among those areas for improvement? Stick to a regular sleep schedule, stay mentally and physically active during the day, create a cool and dark sleep environment, and minimize things like coffee late in the day and screen time before bed. A warm shower before turning in for the night has also been shown to increase the quality of deep, slow-wave sleep, Zavecz said.
With a small sample size of healthy participants, the study is simply an early step in understanding the precise ways sleep may forestall memory loss and the advance of Alzheimer’s, Zavecz said.
Still, it opens the door for potential longer-term experiments examining sleep-enhancement treatments that could have far-reaching implications.
“One of the advantages of this result is the application to a huge population right above the age of 65,” Zavecz said. “By sleeping better and doing your best to practice good sleep hygiene, which is easy to research online, you can gain the benefit of this compensatory function against this type of Alzheimer’s pathology.”
About this Alzheimer’s disease research news
Author: Jason Pohl
Source: UC Berkeley
Contact: Jason Pohl – UC Berkeley
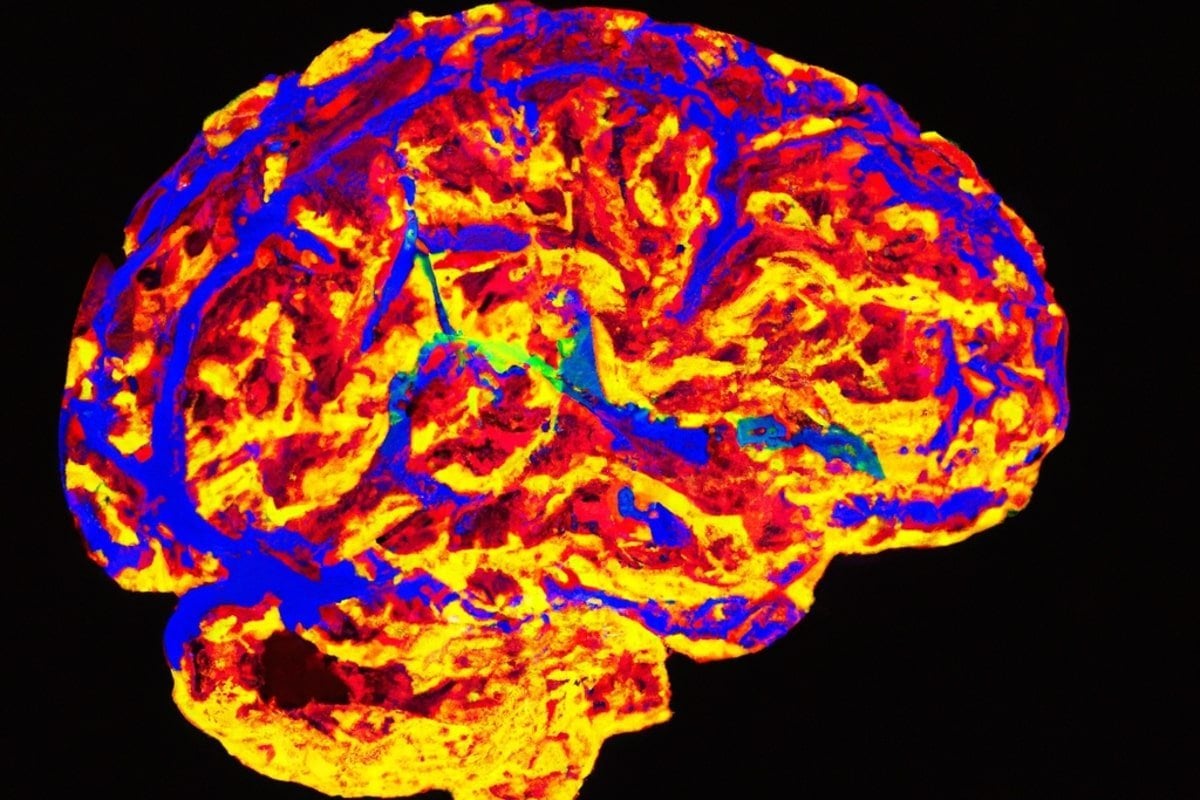
Image: The image is credited to Neuroscience News
Original Research: Open access.
“NREM sleep as a novel protective cognitive reserve factor in the face of Alzheimer’s disease pathology” by Zsófia Zavecz et al. BMC Medicine
Abstract
NREM sleep as a novel protective cognitive reserve factor in the face of Alzheimer’s disease pathology
Background
Alzheimer’s disease (AD) pathology impairs cognitive function. Yet some individuals with high amounts of AD pathology suffer marked memory impairment, while others with the same degree of pathology burden show little impairment. Why is this? One proposed explanation is cognitive reserve i.e., factors that confer resilience against, or compensation for the effects of AD pathology. Deep NREM slow wave sleep (SWS) is recognized to enhance functions of learning and memory in healthy older adults. However, the quality of NREM SWS (NREM slow wave activity, SWA) represents a novel cognitive reserve factor in older adults with AD pathology, thereby providing compensation against memory dysfunction otherwise caused by high AD pathology burden, remains unknown.
Methods
Here, we tested this hypothesis in cognitively normal older adults (N = 62) by combining 11C-PiB (Pittsburgh compound B) positron emission tomography (PET) scanning for the quantification of β-amyloid (Aβ) with sleep electroencephalography (EEG) recordings to quantify NREM SWA and a hippocampal-dependent face-name learning task.
Results
We demonstrated that NREM SWA significantly moderates the effect of Aβ status on memory function. Specifically, NREM SWA selectively supported superior memory function in individuals suffering high Aβ burden, i.e., those most in need of cognitive reserve (B = 2.694, p = 0.019). In contrast, those without significant Aβ pathological burden, and thus without the same need for cognitive reserve, did not similarly benefit from the presence of NREM SWA (B = -0.115, p = 0.876). This interaction between NREM SWA and Aβ status predicting memory function was significant after correcting for age, sex, Body Mass Index, gray matter atrophy, and previously identified cognitive reserve factors, such as education and physical activity (p = 0.042).
Conclusions
These findings indicate that NREM SWA is a novel cognitive reserve factor providing resilience against the memory impairment otherwise caused by high AD pathology burden. Furthermore, this cognitive reserve function of NREM SWA remained significant when accounting both for covariates and factors previously linked to resilience, suggesting that sleep might be an independent cognitive reserve resource. Beyond such mechanistic insights are potential therapeutic implications. Unlike many other cognitive reserve factors (e.g., years of education, and prior job complexity), sleep is a modifiable factor. As such, it represents an intervention possibility that may aid the preservation of cognitive function in the face of AD pathology, both present moment and longitudinally.
